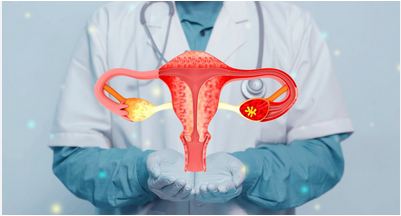
Endometriosis is a common yet often misunderstood women’s health condition that affects millions of people worldwide. Despite its prevalence, many individuals live for years without a proper diagnosis, believing their symptoms are “normal” or something they must simply endure. Raising awareness about endometriosis is essential for early detection, better treatment, and improved quality of life.
1. What Is Endometriosis?
Endometriosis occurs when tissue similar to the lining of the uterus (called endometrial tissue) grows outside the uterus. These growths are commonly found on the ovaries, fallopian tubes, pelvic walls, and sometimes even the bladder or intestines.
Unlike normal uterine lining, which sheds during menstruation, this misplaced tissue has no way to exit the body. As a result, it becomes inflamed, irritated, and can cause pain, swelling, and scar tissue. Over time, this can lead to adhesions—where organs stick together—and chronic discomfort.
Endometriosis is considered a chronic condition, meaning it usually requires long-term management rather than a one-time treatment.
2. How Common Is Endometriosis?
Endometriosis affects approximately 1 in 10 women and people with uteruses of reproductive age. However, the true number may be even higher, as many cases go undiagnosed.
One of the biggest challenges is that symptoms can vary widely. Some individuals experience severe pain, while others may have few or no noticeable symptoms at all.
3. Common Symptoms of Endometriosis
Symptoms of endometriosis differ from person to person, but the most common include:
-
Painful periods that interfere with daily life
-
Chronic pelvic or lower back pain
-
Pain during or after intercourse
-
Heavy or irregular menstrual bleeding
-
Painful bowel movements or urination
-
Bloating, nausea, or digestive issues
-
Fatigue and low energy
-
Difficulty getting pregnant
It’s important to note that the severity of pain does not always reflect the severity of the condition. Someone with mild endometriosis may experience intense pain, while another person with extensive tissue growth may feel very little discomfort.
4. What Causes Endometriosis?
The exact cause of endometriosis is still not fully understood, but researchers believe several factors may contribute:
1. Retrograde Menstruation
This occurs when menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body.
2. Genetic Factors
Endometriosis often runs in families, suggesting a hereditary component.
3. Immune System Issues
A weakened or altered immune response may fail to eliminate misplaced tissue.
4. Hormonal Imbalance
Estrogen appears to play a role in promoting tissue growth.
While these theories help explain the condition, there is currently no known way to prevent endometriosis.
5. How Is Endometriosis Diagnosed?
Diagnosing endometriosis can be challenging. Many people wait 7–10 years before receiving an accurate diagnosis because symptoms are often mistaken for regular menstrual pain.
Doctors may use:
-
Pelvic exams
-
Ultrasound or MRI scans
-
Medical history and symptom tracking
However, the only definitive way to diagnose endometriosis is through a minor surgical procedure called laparoscopy, where a small camera is inserted into the abdomen to directly observe and sample tissue.
6. Treatment Options for Endometriosis
There is no cure for endometriosis, but several treatments can help manage symptoms and slow progression.
1. Pain Management
Over-the-counter medications like ibuprofen or acetaminophen can help reduce mild pain.
2. Hormonal Therapy
Birth control pills, hormonal patches, or hormone-suppressing medications can reduce menstrual flow and limit tissue growth.
3. Surgery
Laparoscopic surgery may be used to remove or destroy endometrial tissue. This often improves pain and fertility outcomes.
4. Lifestyle Support
While not a replacement for medical care, healthy habits may help manage symptoms:
-
Balanced nutrition
-
Regular physical activity
-
Stress reduction
-
Adequate sleep
7. Endometriosis and Fertility
Endometriosis is one of the leading causes of infertility. The condition can interfere with egg release, fertilization, and implantation.
However, many individuals with endometriosis do conceive naturally or with medical support. Early diagnosis and appropriate treatment greatly improve fertility outcomes.
8. Emotional and Mental Health Impact
Living with chronic pain can affect mental well-being. Many people with endometriosis experience:
-
Anxiety
-
Depression
-
Frustration or isolation
-
Difficulty concentrating at school or work
Because symptoms are often invisible, individuals may feel misunderstood or dismissed. Support from healthcare providers, family, and peer communities plays a vital role in emotional resilience.
9. Why Awareness Matters
Endometriosis is often normalized as “just bad periods,” which delays care and increases suffering. Greater awareness helps:
-
Reduce diagnostic delays
-
Improve access to treatment
-
Validate patient experiences
-
Encourage research and funding
When people recognize that severe menstrual pain is not normal, they are more likely to seek help early.
10. Living Well With Endometriosis
Although endometriosis can be life-altering, many individuals learn to manage their symptoms and live full, active lives. The key is:
-
Listening to your body
-
Seeking professional care
-
Tracking symptoms
-
Advocating for yourself
With proper support, education, and medical guidance, endometriosis does not have to define one’s future.
Final Thoughts
Endometriosis is a widespread yet under-recognized health condition that deserves more attention, research, and compassion. By shedding light on its symptoms, causes, and treatment options, we empower individuals to take control of their health and seek the care they deserve.
Understanding endometriosis is not just a medical issue—it’s a step toward better quality of life, equality in healthcare, and informed self-advocacy for millions around the world.































Discussion about this post